
“I haven’t yet gotten over the trauma of the first wave, the second, or the third, and here I am again treating COVID-19 patients,” said Ahlam Abu Hamida, a nurse at the Galilee Medical Center in Nahariya, which is Israel’s second-largest hospital in the north.
Half of the rehabilitation ward where Abu Hamida works was converted to treat COVID-19 patients in need of respiratory support. Officially, she is responsible for caring for patients in rehabilitation, but in practice she spends her days on the other side of the ward, surrounded by difficult memories.
“I move between the rooms of the ward, and in every room I am reminded of patients I cared for and who passed in the previous waves,” Abu Hamida said.

“Death in this ward isn’t like death in other wards,” Abu Hamida said. “It’s different. It isn’t like other patients who can see and hear you. The disconnection from the family, even when they know that death is coming, it’s really hard.”
Abu Hamida and the rest of the staff in Corona Ward B and the Respiratory Corona Ward described in conversations with Davar increasing feelings of burnout, trauma, and fear, brought about from a lack of staff as well as intense physical and emotional labor.
“There isn’t enough staff, we’re doing what we can”
The number of COVID-19 hospitalizations at the Galilee Medical Center has increased dramatically and forced the hospital to open an additional COVID-19 ward. As of the publication of this article, the hospital has two COVID-19 wards at full capacity, the first of which reopened four weeks ago, and half a ward that has been converted to treat COVID-19 patients with respiratory problems.
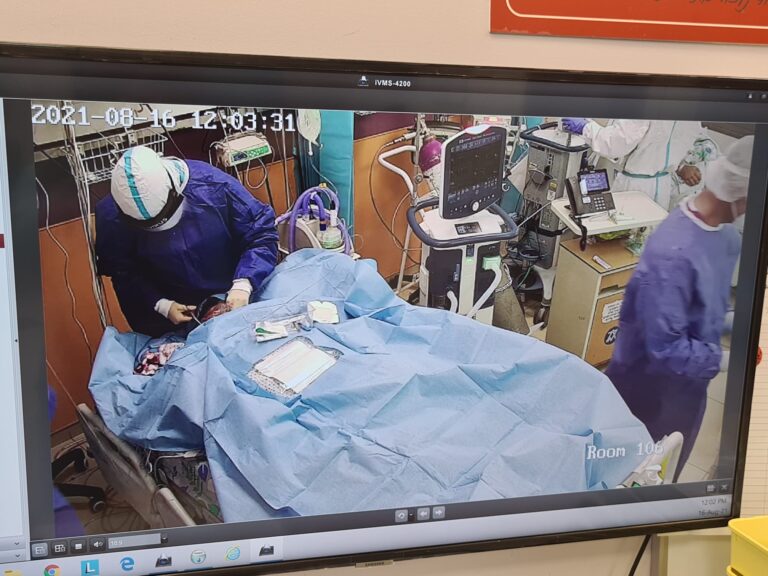
In Corona Ward B, the serious shortage of medical personnel is palpable: only four nurses are around to treat 21 patients, some of whom require invasive respiratory support and maximum supervision. New hospital staff have not been brought on in pace with the number of new patients filling the ward. At noon, a doctor, an intern, and a nurse worked together to examine a patient who was in severe mental distress. The other nurses in the ward sat in the ward’s situation room, attending to the screens listing numerous other patients.
“We’re four nurses with so many patients and a lot of action going on,” said Marwan Arshid, a nurse in the ward. “We escort patients to a CT scan, give plasma treatment and Remdesivir [an antiviral medication used to treat COVID-19], a treatment that we’re still overburdened by.”

Arshid expressed frustration with the disconnect between the harrowing reality in the ward and the relatively lenient policy pursued by the government with regard to COVID-19 restrictions, which she suspects will lead to additional COVID-19 patients.
“It’s atrocious. And there isn’t a lockdown, there are no guidelines, the floodgates have opened, and everyone is out celebrating. It’s going to exacerbate and increase the burden on us even more,” Arshid said.
The remarks of the healthcare professionals on the ground call into question the announcements of Prime Minister Naftali Bennett and Health Minister Nitzan Horowitz regarding their intention to immediately hire hundreds of healthcare workers in hospitals across Israel. Despite these promises, the hospital has not yet been instructed to take on new staff — and those who serve in the ward are split as to whether new hires will be the panacea it’s been promised to be.
Dr. Getas Nasser, Director of Internal Medicine in the Corona B ward, expressed gratitude for the planned reinforcements and hope that they would be arriving soon. “I hope they will offer backup for my staff,” he said.
“I really appreciate the Minister of Health and the Prime Minister for initiating the third vaccine. But the mental and physical burden on the staff is huge. Working in a protective suit [everday] is not easy and we deal with patients who die before our eyes.”
On the other hand, Irina Siderovski, the deputy nurse in charge of the ward, was pessimistic about the extent to which temporary staff increases can ease the burden on the ward’s healthcare workers. These reinforcements are intended to address the increasing numbers of patients, but staff have been overworked and unable to carry out all their duties even before the patient numbers started to tick back up. And when medical staff from other wards came to provide backup, they often don’t have the necessary experience to take on the required duties.
“The nurses wear protective gear for four hours straight. We have complicated patients here who demand a lot. There isn’t enough staff and we are doing everything we can,” Siderovski said.
“The hospital is trying to support us and send more staff, but care for COVID-19 patients is complex, and there is a limit to what staff from other professions can do.
“We released 31 patients within a week when we were instructed to re-open the COVID-19 ward, and the ward filled up pretty quickly. The teams remove their protective gear once they’re exhausted, and many times they need to put it on again twice or more over the course of their shifts. For instance, patients who are disoriented by lack of oxygen remove their oxygen tubes, and then the staff need to quickly put on protective clothing, reconnect the oxygen, calm the patients down and explain the situation to them again.”
According to Siderovski, the current wave may call for an even higher staff-to-patient ratio. “I think that as a result of the Delta variant, the deterioration of patients in this wave is quicker,” Siderovski said. “This also contributes to our load — there needs to be 200 eyes on a patient in order to catch the deterioration in time to bring it to the doctor’s attention so that they can intervene with oxygen. The average age of a hospitalized patient is over 60, but there is also a 19-year-old youth in critical condition.”
The staff’s responsibilities also extend beyond patients’ medical needs. “The work here is also social work. There are also professional social workers here, but we’re all swept up in it. Comforting phone calls to patients’ families, since the families are allowed to come only once a day and it’s difficult for them. Families tell us that the patients aren’t communicating with them, and ask that we check that their telephone is charged — or to bring the patient a cup of tea or a bottle of water,” Siderovski said.
“We thought that we’d have a little time to breathe”
Siderovski also described the difficulty of returning to caring for COVID-19 patients after having previously closed down the ward. “We were already a COVID-19 ward, we closed [the ward] at the end of April, and opened again as a regular internal ward. We thought that we’d have a little time to catch some air, we didn’t imagine that within a few months we’d need to open up again,” Siderovski said.
“It’s like déjà vu,” said Dr. Dua Saman, an anesthesiologist in the COVID-19 intensive care unit. “We put it behind us. There are motions that were once automatic and now we need to remember them, ways of moving the body with the personal protection equipment that take me back to that time. It’s really hard.”
Part of the staff’s fear stems from the hospitalization of patients who had already been vaccinated or recovered from the disease. “A patient who was hospitalized here in the previous wave came through again,” Siderovski said. “The family called and said, ‘we know you and know that you give dedicated care, we can’t visit because we’re in isolation — look after him, please.’
“It’s hard to hear, and it brings up anxiety that you might get infected — we’re vaccinated, but we see previously vaccinated people coming to us in critical condition. I’m really afraid for my family, though they’re all vaccinated, including my 12-year-old daughter. My mother still shows symptoms even half a year after the illness.”
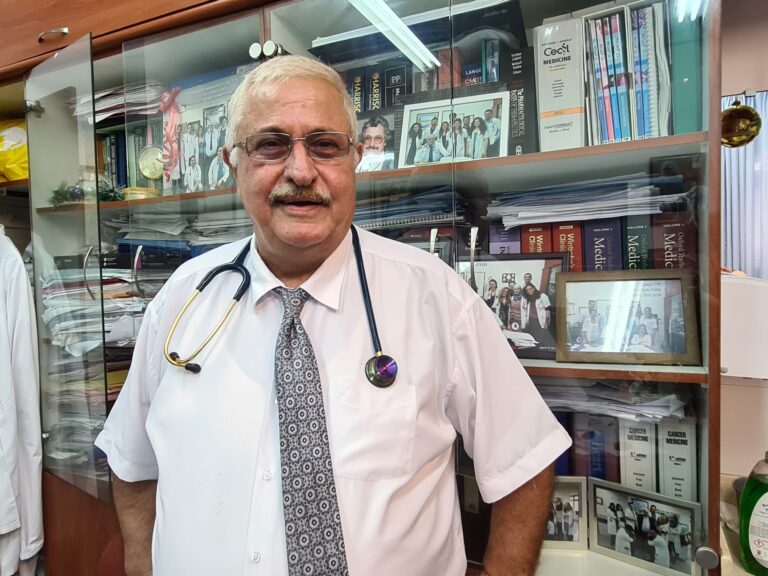
But Nasser made clear that vaccinated Israelis are still in a much better position than the unvaccinated. “It is very important to me that people know that the patients who have not been vaccinated go through a much more difficult clinical process than the patients who have been vaccinated,” said Nasser. According to him, out of 50 patients who went through the ward, there was only one who had received a third dose of the vaccine who regardless was in critical condition. Of the four critically ill patients transferred from the COVID-19 ward to the intensive care unit, only one was vaccinated.






